Page 7 - Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH): 2018 update
P. 7
Guideline: Male LUTS/BPH
local anaesthetic), mechanical, stent-like device designed Algorithms summarizing the management of a patient
to remodel the bladder neck and the prostatic urethra with MLUTS/BPH are summarized in Figs. 2, 3.
through pressure necrosis. Early clinical experience dem-
onstrated that implantation of iTIND is a feasible and safe 2.5. Special situations
procedure to perform and appears to provide measureable
clinical benefit. 74 2.5.1. Symptomatic prostatic enlargement without bothersome symptoms
We recommend that iTIND should not be offered at this Studies have shown that 5ARIs prevent progression of
time for the treatment of LUTS due to BPH (conditional MLUTS/BPH in symptomatic men over the long-term. 28,29
recommendation based on very low-quality evidence). We suggest that selected, well-informed patients with
Prostatic artery embolization (PAE): PAE, exclusively per- symptomatic prostatic enlargement in the absence of sig-
formed by interventional radiologists at specialized centres, nificant bother may be offered a 5ARI to prevent progres-
results in significant IPSS, Qmax, and PVR improvement sion of the disease (conditional recommendation based on
75
compared to baseline at 12 months, however, inferior moderate-quality evidence).
79
outcomes compared to TURP 76-78 or OSP. Non-targeted AUR: Data suggest that in patients with AUR, the use
embolization may lead to ischemic complications like alpha-blockers (specifically tamsulosin, alfuzosin, and
transient ischemic proctitis, bladder ischemia, urethral and silodosin) during the period of catheterization will increase
ureteral stricture, or seminal vesicles ischemia. the chances of successful voiding after catheter removal, 80,81
We recommend that PAE should not be offered at this while the addition of a 5ARI may decrease the risk of future
time for the treatment of LUTS due to BPH (conditional prostate surgery. 28,29,82
recommendation based on moderate-quality evidence). We suggest that men with AUR secondary to BPH
may be offered alpha-blocker
therapy during the period of
Male LUTS: catheterization (conditional
-With absolute indications for BPH surgery recommendation based on
or
moderate-quality evidence).
-Those who do not want medical treatment but request active treatment
Detrusor underactivity
(DU): There is no effective
LOW Medical risk HIGH treatment for DU, defined
as a contraction of reduced
Fit to undergo
YES NO strength and/or duration,
anesthesia?
resulting in prolonged blad -
Able to discontinue antiplatelet/ der emptying and/or a failure
anticoagulation medication
to achieve complete bladder
Prostate
volume YES NO emptying within a normal
time span. In primary DU,
83
treatment approach should
be to facilitate bladder empty-
<30 cc 30–80 cc >80 cc
ing, identify agents that can
decrease bladder contractility,
• TUIP* • M/B-TURP* • OSP* • Greenlight PVP* • TUMT**
• M/B-TURP • Greenlight PVP • HoLEP • HoLEP • Urolift** or increase urethral resistance.
• Urolift** • HoLEP • Greenlight PVP • Thulium laser • Rezum
• BPKVP • Thulium laser vaporization/ • Urethral stent Behavioural modification,
• Thulium laser vaporization/ enucleation including scheduled voiding
vaporization enucleation
• Diode laser • B-TURP and or double voiding, clean
vaporization • Aquablation
• Urolift** intermittent self-catheterization
• Rezum (CIC), or indwelling catheters,
• TUMT**
84
• Aquablation are optional strategies. The
data suggests that DU is not
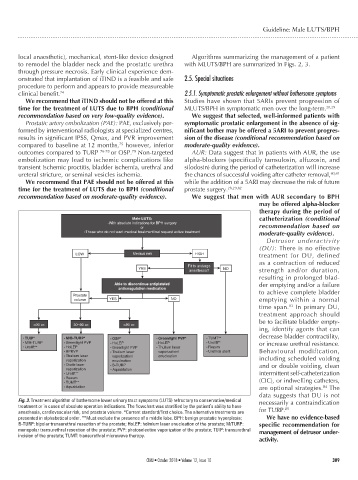
Fig. 3. Treatment algorithm of bothersome lower urinary tract symptoms (LUTS) refractory to conservative/medical necessarily a contraindication
treatment or in cases of absolute operation indications. The flowchart was stratified by the patient’s ability to have 85
anesthesia, cardiovascular risk, and prostate volume. *Current standard/first choice. The alternative treatments are for TURP.
presented in alphabetical order. **Must exclude the presence of a middle lobe. BPH: benign prostatic hyperplasia; We have no evidence-based
B-TURP: bipolar transurethral resection of the prostate; HoLEP: holmium laser enucleation of the prostate; M/TURP: specific recommendation for
monopolar transurethral resection of the prostate; PVP: photoselective vaporization of the prostate; TUIP: transurethral management of detrusor under-
incision of the prostate; TUMT: transurethral microwave therapy.
activity.
CUAJ • October 2018 • Volume 12, Issue 10 309