Page 6 - Diagnosis, management, and surveillance of neurogenic lower urinary tract dysfunction – Full text
P. 6
Kavanagh et al
Focused history, physical exam, PVR, and UA
SCI, spina bifida, advanced MS Other neurological diseases
All *Selected patients Most
Baseline UDS, renal US, renal function
Optimize bladder
Determine if risk factors are management technique,
present based on: incontinence, urinary
1. Bladder management symptoms, and UTI risk
2. UDS
3. Renal US
4. Renal fuction
High-risk Moderate-risk Low-risk
*Clinically significant PVR
Treatment & Optimization Bothersome incontinence
Frequent UTIs
Use of catheters for bladder management
Known high-risk features
Considering more invasive management options
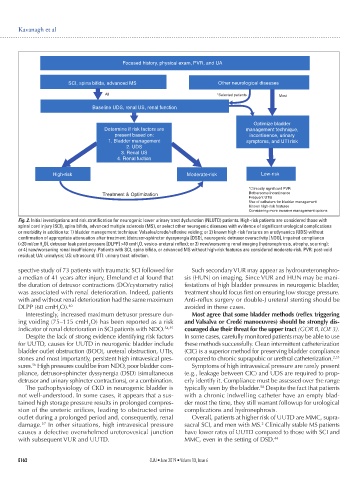
Fig. 2. Initial investigations and risk stratification for neurogenic lower urinary tract dysfunction (NLUTD) patients. High-risk patients are considered those with
spinal cord injury (SCI), spina bifida, advanced multiple sclerosis (MS), or select other neurogenic diseases with evidence of significant urological complications
or morbidity in addition to: 1) bladder management technique: Valsalva/crede/reflexive voiding; or 2) known high-risk features on urodynamics (UDS) without
confirmation of appropriate attenuation after treatment (detrusor-sphincter dyssynergia [DSD], neurogenic detrusor overactivity [NDO], impaired compliance
(<20 ml/cmH O), detrusor leak point pressure [DLPP] >40 cmH O, vesico-ureteral reflex); or 3) new/worsening renal imaging (hydronephrosis, atrophy, scarring);
2
2
or 4) new/worsening renal insufficiency. Patients with SCI, spina bifida, or advanced MS without high-risk features are considered moderate-risk. PVR: post-void
residual; UA: urinalysis; US: ultrasound; UTI: urinary tract infection.
spective study of 73 patients with traumatic SCI followed for Such secondary VUR may appear as hydroureteronephro-
a median of 41 years after injury, Elmelund et al found that sis (HUN) on imaging. Since VUR and HUN may be mani-
the duration of detrusor contractions (DO/cystometry ratio) festations of high bladder pressures in neurogenic bladder,
was associated with renal deterioration. Indeed, patients treatment should focus first on ensuring low storage pressure.
with and without renal deterioration had the same maximum Anti-reflux surgery or double-J ureteral stenting should be
DLPP (60 cmH O). 40 avoided in these cases.
2
Interestingly, increased maximum detrusor pressure dur- Most agree that some bladder methods (reflex triggering
ing voiding (75–115 cmH O) has been reported as a risk and Valsalva or Credé manoeuvres) should be strongly dis-
2
indicator of renal deterioration in SCI patients with NDO. 54,55 couraged due their threat for the upper tract (GOR B, LOE 3).
Despite the lack of strong evidence identifying risk factors In some cases, carefully monitored patients may be able to use
for UUTD, causes for UUTD in neurogenic bladder include these methods successfully. Clean intermittent catheterization
bladder outlet obstruction (BOO), ureteral obstruction, UTIs, (CIC) is a superior method for preserving bladder compliance
stones and most importantly, persistent high intravesical pres- compared to chronic suprapubic or urethral catheterization. 2,33
sures. High pressures could be from NDO, poor bladder com- Symptoms of high intravesical pressure are rarely present
56
pliance, detrusor-sphincter dyssynergia (DSD) (simultaneous (e.g., leakage between CIC) and UDS are required to prop-
detrusor and urinary sphincter contractions), or a combination. erly identify it. Compliance must be assessed over the range
58
The pathophysiology of CKD in neurogenic bladder is typically seen by the bladder. Despite the fact that patients
not well-understood. In some cases, it appears that a sus- with a chronic indwelling catheter have an empty blad-
tained high storage pressure results in prolonged compres- der most the time, they still warrant followup for urological
sion of the ureteric orifices, leading to obstructed urine complications and hydronephrosis.
outlet during a prolonged period and, consequently, renal Overall, patients at higher risk of UUTD are MMC, supra-
2
57
damage. In other situations, high intravesical pressure sacral SCI, and men with MS. Clinically stable MS patients
causes a defective overwhelmed ureterovesical junction have lower rates of UUTD compared to those with SCI and
with subsequent VUR and UUTD. MMC, even in the setting of DSD. 44
E162 CUAJ • June 2019 • Volume 13, Issue 6