Page 1 - CUA 2020_Endourology
P. 1
2020 CUA ABSTRACTS
Podium Session 1: Endourology, Nephrolithiasis
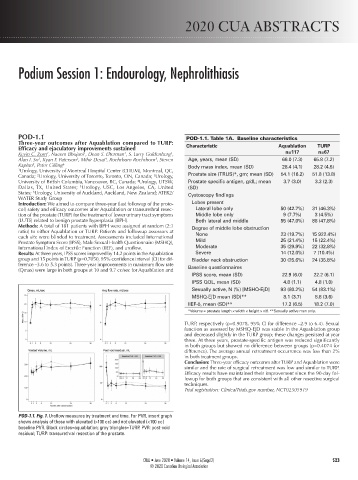
POD-1.1 POD-1.1. Table 1A. Baseline characteristics
Three-year outcomes after Aquablation compared to TURP:
Efficacy and ejaculatory improvements sustained Characteristic Aquablation TURP
3
2
1
1
Kevin C. Zorn , Naeem Bhojani , Dean S. Elterman , S. Larry Goldenberg , n=117 n=67
Alan I. So , Ryan F. Paterson , Mihir Desai , Roehrborn Roehrborn , Steven Age, years, mean (SD) 66.0 (7.3) 65.8 (7.2)
3
3
4
5
Kaplan , Peter Gilling 6 Body mass index, mean (SD) 28.4 (4.1) 28.2 (4.5)
5
1 Urology, University of Montreal Hospital Center (CHUM), Montreal, QC,
3
2
Canada; Urology, University of Toronto, Toronto, ON, Canada; Urology, Prostate size (TRUS)*, gm; mean (SD) 54.1 (16.2) 51.8 (13.8)
4
University of British Columbia, Vancouver, BC, Canada; Urology, UTSW, Prostate specific antigen, g/dL; mean 3.7 (3.0) 3.3 (2.3)
5
Dallas, TX, United States; Urology, USC, Los Angeles, CA, United (SD)
States; Urology, University of Auckland, Auckland, New Zealand; ATER2/ Cystoscopy findings
6
WATER Study Group
Introduction: We aimed to compare three-year (last followup of the proto- Lobes present
col) safety and efficacy outcomes after Aquablation or transurethral resec- Lateral lobe only 50 (42.7%) 31 (46.3%)
tion of the prostate (TURP) for the treatment of lower urinary tract symptoms Middle lobe only 9 (7.7%) 3 (4.5%)
(LUTS) related to benign prostate hyperplasia (BPH). Both lateral and middle 55 (47.0%) 88 (47.8%)
Methods: A total of 181 patients with BPH were assigned at random (2:1 Degree of middle lobe obstruction
ratio) to either Aquablation or TURP. Patients and followup assessors at None 23 (19.7%) 15 922.4%)
each site were blinded to treatment. Assessments included International
Prostate Symptom Score (IPSS), Male Sexual Health Questionnaire (MSHQ), Mild 25 (21.4%) 15 (22.4%)
International Index of Erectile Function (IIEF), and uroflow. Moderate 35 (29.9%) 22 (32.8%)
Results: At three years, IPSS scores improved by 14.2 points in the Aquablation Severe 14 (12.0%) 7 (10.4%)
group and 15 points in TURP (p=0.7050, 95% confidence interval [CI] for dif- Bladder neck obstruction 30 (25.6%) 24 (35.8%)
ference –3.6 to 5.3 points). Three-year improvements in maximum flow rate Baseline questionnaires
(Qmax) were large in both groups at 10 and 9.7 cc/sec for Aquablation and
IPSS score, mean (SD) 22.9 (6.0) 22.2 (6.1)
IPSS QOL, mean (SD) 4.8 (1.1) 4.8 (1.0)
Sexually active, N (%) [MSHQ-EjD] 93 (80.2%) 54 (83.1%)
MSHQ-EjD mean (SD)** 8.1 (3.7) 8.8 (3.6)
IIEF-5, mean (SD)** 17.2 (6.5) 18.2 (7.0)
*Volume = prostate length × width × height × π/6. **Sexually active men only.
TURP, respectively (p=0.9078, 95% CI for difference –2.9 to 6.4). Sexual
function as assessed by MSHQ-EjD was stable in the Aquablation group
and decreased slightly in the TURP group; these changes persisted at year
three. At three years, prostate-specific antigen was reduced significantly
in both groups but showed no difference between groups (p=0.4074 for
difference). The average annual retreatment occurrence was less than 2%
in both treatment groups.
Conclusion: Three-year efficacy outcomes after TURP and Aquablation were
similar and the rate of surgical retreatment was low and similar to TURP.
Efficacy results have maintained their improvement since the 90-day fol-
lowup for both groups that are consistent with all other resective surgical
techniques.
Trial registration: ClinicalTrials.gov number, NCT02505919
POD-1.1. Fig. 1. Uroflow measures by treatment and time. For PVR, insert graph
shows analysis of those with elevated (>100 cc) and not elevated (<100 cc)
baseline PVR. Black circles=aquablation; gray triangles=TURP. PVR: post-void
residual; TURP: transurethral resection of the prostate.
CUAJ • June 2020 • Volume 14, Issue 6(Suppl2) S23
© 2020 Canadian Urological Association