Page 86 - CUA Absracts 2022_Fulldraft
P. 86
2022 CUA Abstracts
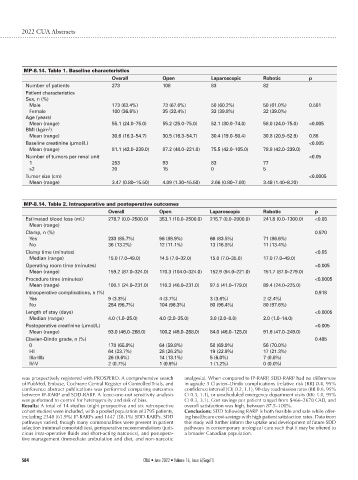
MP-8.14. Table 1. Baseline characteristics
Overall Open Laparoscopic Robotic p
Number of patients 273 108 83 82
Patient characteristics
Sex, n (%)
Male 173 (63.4%) 73 (67.6%) 50 (60.2%) 50 (61.0%) 0.501
Female 100 (36.6%) 35 (32.4%) 33 (39.8%) 32 (39.0%)
Age (years)
Mean (range) 55.1 (24.0–75.0) 55.2 (25.0–75.0) 52.1 (30.0–74.0) 58.0 (24.0–75.0) <0.005
BMI (kg/m )
2
Mean (range) 30.6 (16.3–54.7) 30.5 (16.3–54.7) 30.4 (19.0–50.4) 30.8 (20.9–52.9) 0.88
Baseline creatinine (μmol/L) <0.005
Mean (range) 81.1 (42.0–239.0) 87.2 (48.0–221.0) 75.5 (42.0–105.0) 78.8 (42.0–239.0)
Number of tumors per renal unit <0.05
1 253 93 83 77
≥2 20 15 0 5
Tumor size (cm) <0.0005
Mean (range) 3.47 (0.80–15.50) 4.09 (1.30–15.50) 2.66 (0.80–7.00) 3.48 (1.40–8.20)
MP-8.14. Table 2. Intraoperative and postoperative outcomes
Overall Open Laparoscopic Robotic p
Estimated blood loss (mL) 278.7 (0.0–2500.0) 353.1 (10.0–2500.0) 215.7 (0.0–2000.0) 241.8 (0.0–1300.0) <0.05
Mean (range)
Clamp, n (%) 0.570
Yes 233 (85.7%) 96 (88.9%) 66 (83.5%) 71 (86.6%)
No 36 (13.2%) 12 (11.1%) 13 (16.5%) 11 (13.4%)
Clamp time (minutes) <0.05
Median (range) 15.0 (7.0–49.0) 14.5 (7.0–32.0) 15.0 (7.0–35.0) 17.0 (7.0–49.0)
Operating room time (minutes) <0.005
Mean (range) 159.2 (87.0–324.0) 170.3 (104.0–324.0) 152.9 (94.0–221.0) 151.7 (87.0–279.0)
Procedure time (minutes) <0.0005
Mean (range) 100.1 (24.0–231.0) 110.3 (40.0–231.0) 97.5 (41.0–179.0) 89.4 (24.0–225.0)
Intraoperative complications, n (%) 0.918
Yes 9 (3.3%) 4 (3.7%) 3 (3.6%) 2 (2.4%)
No 264 (96.7%) 104 (96.3%) 80 (96.4%) 80 (97.6%)
Length of stay (days) <0.0005
Median (range) 4.0 (1.0–25.0) 4.0 (2.0–25.0) 3.0 (2.0–8.0) 2.0 (1.0–14.0)
Postoperative creatinine (μmol/L) <0.005
Mean (range) 93.0 (46.0–268.0) 100.2 (49.0–268.0) 84.0 (46.0–125.0) 91.6 (47.0–249.0)
Clavien-Dindo grade, n (%) 0.485
0 178 (65.9%) 64 (59.8%) 58 (69.9%) 56 (70.0%)
I-II 64 (23.7%) 28 (26.2%) 19 (22.9%) 17 (21.3%)
IIIa-IIIb 26 (9.6%) 14 (13.1%) 5 (6.0%) 7 (8.8%)
IV-V 2 (0.7%) 1 (0.9%) 1 (1.2%) 0 (0.0%)
was prospectively registered with PROSPERO. A comprehensive search analgesia). When compared to IP-RARP, SDD-RARP had no differences
of PubMed, Embase, Cochrane Central Register of Controlled Trials, and in ≥grade 3 Clavien–Dindo complications (relative risk [RR] 0.4, 95%
conference abstract publications was performed comparing outcomes confidence interval [CI] 0.2, 1.1), 90-day readmission rates (RR 0.6, 95%
between IP-RARP and SDD-RARP. A leave-one-out sensitivity analysis CI 0.3, 1.1), or unscheduled emergency department visits (RR: 1.0, 95%
was performed to control for heterogeneity and risk of bias. CI 0.3, 3.1). Cost savings per patient ranged from $466–2678 CAD, and
Results: A total of 14 studies (eight prospective and six retrospective overall satisfaction was high, between 87.5–100%.
cohort studies) were included, with a pooled population of 3795 patients, Conclusions: SDD following RARP is both feasible and safe while offer-
including 2348 (61.9%) IP-RARPs and 1447 (38.1%) SDD-RARPs. SDD ing healthcare cost-savings with high patient satisfaction rates. Data from
pathways varied, though many commonalities were present in patient this study will further inform the uptake and development of future SDD
selection (minimal comorbidities), perioperative recommendations (judi- pathways in contemporary urological care such that it may be offered to
cious intra-operative fluids and short-acting narcotics), and postopera- a broader Canadian population.
tive management (immediate ambulation and diet, and non-narcotic
S84 CUAJ • June 2022 • Volume 16, Issue 6(Suppl1)