Page 16 - CUAJFeb2023
P. 16
Rowe et al
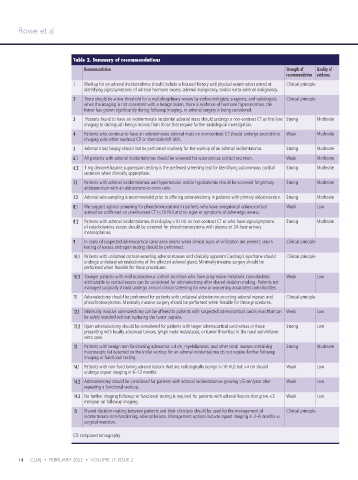
Table 2. Summary of recommendations
Recommendation Strength of Quality of
recommendation evidence
1 Workup for an adrenal incidentaloma should include a focused history and physical examination aimed at Clinical principle
identifying signs/symptoms of adrenal hormone excess, adrenal malignancy, and/or extra-adrenal malignancy.
2 There should be a low threshold for a multidisciplinary review by endocrinologists, surgeons, and radiologists Clinical principle
when the imaging is not consistent with a benign lesion, there is evidence of hormone hypersecretion, the
tumor has grown significantly during followup imaging, or adrenal surgery is being considered.
3 Patients found to have an indeterminate incidental adrenal mass should undergo a non-contrast CT as first-line Strong Moderate
imaging to distinguish benign lesions from those that require further radiological investigation.
4 Patients who continue to have an indeterminate adrenal mass on non-contrast CT should undergo second-line Weak Moderate
imaging with either washout CT or chemical-shift MRI.
5 Adrenal mass biopsy should not be performed routinely for the workup of an adrenal incidentaloma. Strong Moderate
6.1 All patients with adrenal incidentalomas should be screened for autonomous cortisol secretion. Weak Moderate
6.2 1 mg dexamethasone suppression testing is the preferred screening test for identifying autonomous cortisol Strong Moderate
secretion when clinically appropriate.
7.1 Patients with adrenal incidentalomas and hypertension and/or hypokalemia should be screened for primary Strong Moderate
aldosteronism with an aldosterone-to-renin ratio.
7.2 Adrenal vein sampling is recommended prior to offering adrenalectomy in patients with primary aldosteronism. Strong Moderate
8.1 We suggest against screening for pheochromocytoma in patients who have unequivocal adrenocortical Weak Low
adenomas confirmed on unenhanced CT (<10 HU) and no signs or symptoms of adrenergic excess.
8.2 Patients with adrenal incidentalomas that display ≥10 HU on non-contrast CT or who have signs/symptoms Strong Moderate
of catecholamine excess should be screened for pheochromocytoma with plasma or 24-hour urinary
metanephrines.
9 In cases of suspected adrenocortical carcinoma and/or when clinical signs of virilization are present, serum Clinical principle
testing of excess androgen testing should be performed.
10.1 Patients with unilateral cortisol-secreting adrenal masses and clinically apparent Cushing's syndrome should Clinical principle
undergo unilateral adrenalectomy of the affected adrenal gland. Minimally invasive surgery should be
performed when feasible for these procedures.
10.2 Younger patients with mild autonomous cortisol secretion who have progressive metabolic comorbidities Weak Low
attributable to cortisol excess can be considered for adrenalectomy after shared decision-making. Patients not
managed surgically should undergo annual clinical screening for new or worsening associated comorbidities.
11 Adrenalectomy should be performed for patients with unilateral aldosterone-secreting adrenal masses and Clinical principle
pheochromocytomas. Minimally invasive surgery should be performed when feasible for these procedures.
12.1 Minimally invasive adrenalectomy can be offered to patients with suspected adrenocortical carcinomas that can Weak Low
be safely resected without rupturing the tumor capsule.
12.2 Open adrenalectomy should be considered for patients with larger adrenocortical carcinomas or those Strong Low
presenting with locally advanced tumors, lymph node metastases, or tumor thrombus in the renal vein/inferior
vena cava.
13 Patients with benign non-functioning adenomas <4 cm, myelolipomas, and other small masses containing Strong Moderate
macroscopic fat detected on the initial workup for an adrenal incidentaloma do not require further followup
imaging or functional testing.
14.1 Patients with non-functioning adrenal lesions that are radiologically benign (<10 HU) but >4 cm should Weak Low
undergo repeat imaging in 6–12 months
14.2 Adrenalectomy should be considered for patients with adrenal incidentalomas growing >5 mm/year after Weak Low
repeating a functional workup.
14.3 No further imaging followup or functional testing is required for patients with adrenal lesions that grow <3 Weak Low
mm/year on followup imaging.
15 Shared decision-making between patients and their clinicians should be used for the management of Clinical principle
indeterminate non-functioning adrenal lesions. Management options include repeat imaging in 3–6 months vs.
surgical resection.
CT: computed tomography.
14 CUAJ • FEBRUARY 2023 • VOLUME 17, ISSUE 2