Page 9 - Guideline
P. 9
09010:Layout 1 3/18/10 9:26 PM Page E27
Management of testicular germ cell cancer
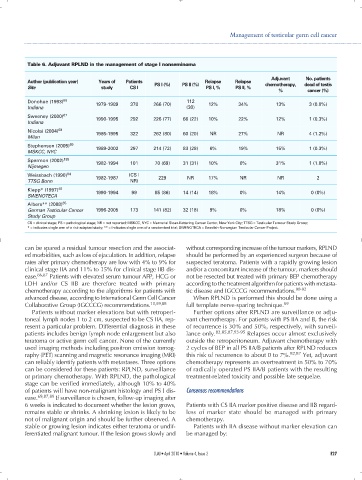
Table 6. Adjuvant RPLND in the management of stage I nonseminoma
Adjuvant No. patients
Author (publication year) Years of Patients PS I (%) PS II (%) Relapse Relapse chemotherapy, dead of testis
Site study CS I PS I, % PS II, %
% cancer (%)
Donohue (1993) 66 1979-1989 378 266 (70) 112 12% 34% 13% 3 (0.8%)
Indiana (30)
Sweeney (2000) 67 1990-1995 292 226 (77) 66 (22) 10% 22% 12% 1 (0.3%)
Indiana
Nicolai (2004) 68
1985-1995 322 262 (80) 60 (20) NR 27% NR 4 (1.2%)
Milan
Stephenson (2005) 69 1989-2002 297 214 (72) 83 (28) 6% 19% 15% 1 (0.3%)
MSKCC, NYC
Spermon (2002) 193
1982-1994 101 70 (69) 31 (31) 10% 0% 31% 1 (1.0%)
Nijmegen
Weissbach (1990) 64 1982-1987 (CS I 229 NR 17% NR NR 2
TTSG Bonn NR)
Klepp* (1997) 48
1990-1994 99 85 (86) 14 (14) 18% 0% 14% 0 (0%)
SWENOTECA
Albers** (2008) 65
German Testicular Cancer 1996-2005 173 141 (82) 32 (18) 9% 0% 18% 0 (0%)
Study Group
CS = clinical stage; PS = pathological stage; NR = not reported; MSKCC, NYC = Memorial Sloan-Kettering Cancer Center, New York City; TTSG = Testicular Tumour Study Group;
* = indicates single arm of a risk-adapted study; ** = indicates single arm of a randomized trial; SWENOTECA = Swedish-Norwegian Testicular Cancer Project.
can be spared a residual tumour resection and the associat- without corresponding increase of the tumour markers, RPLND
ed morbidities, such as loss of ejaculation. In addition, relapse should be performed by an experienced surgeon because of
rates after primary chemotherapy are low with 4% to 9% for suspected teratoma. Patients with a rapidly growing lesion
clinical stage IIA and 11% to 15% for clinical stage IIB dis- and/or a concomitant increase of the tumour, markers should
ease. 86,87 Patients with elevated serum tumour AFP, HCG or not be resected but treated with primary BEP chemotherapy
LDH and/or CS IIB are therefore treated with primary according to the treatment algorithm for patients with metasta-
chemotherapy according to the algorithms for patients with tic disease and IGCCCG recommendations. 90-92
advanced disease, according to International Germ Cell Cancer When RPLND is performed this should be done using a
Collaborative Group (IGCCCG) recommendations. 10,69,88 full template nerve-sparing technique. 69
Patients without marker elevations but with retroperi- Further options after RPLND are surveillance or adju-
toneal lymph nodes 1 to 2 cm, suspected to be CS IIA, rep- vant chemotherapy. For patients with PS IIA and B, the risk
resent a particular problem. Differential diagnosis in these of recurrence is 30% and 50%, respectively, with surveil-
patients includes benign lymph node enlargement but also lance only. 82,85,87,93-95 Relapses occur almost exclusively
teratoma or active germ cell cancer. None of the currently outside the retroperitoneum. Adjuvant chemotherapy with
used imaging methods including positron emission tomog- 2 cycles of BEP in all PS IIA/B patients after RPLND reduces
raphy (PET) scanning and magnetic resonance imaging (MRI) this risk of recurrence to about 0 to 7%. 82,87 Yet, adjuvant
can reliably identify patients with metastases. Three options chemotherapy represents an overtreatment in 50% to 70%
can be considered for these patients: RPLND, surveillance of radically operated PS IIA/B patients with the resulting
or primary chemotherapy. With RPLND, the pathological treatment-related toxicity and possible late sequelae.
stage can be verified immediately, although 10% to 40%
of patients will have non-malignant histology and PS I dis- Consensus recommendations
ease. 69,87,89 If surveillance is chosen, follow-up imaging after
6 weeks is indicated to document whether the lesion grows, Patients with CS IIA marker positive disease and IIB regard-
remains stable or shrinks. A shrinking lesion is likely to be less of marker state should be managed with primary
not of malignant origin and should be further observed. A chemotherapy.
stable or growing lesion indicates either teratoma or undif- Patients with IIA disease without marker elevation can
ferentiated malignant tumour. If the lesion grows slowly and be managed by:
CUAJ • April 2010 • Volume 4, Issue 2 E27